
Amit Mandal
Department of Cardiology Christian Medical College Vellore.
*Corresponding Author: Amit Mandal, Department of Cardiology Christian Medical College Vellore.
Received Date : September 07, 2023
Accepted Date: October 15, 2023
Published Date: November 20, 2023
Citation: Amit Mandal (2023) “ Prosthetic Valve Endocarditis Due to Candida Parapsilosis: A Rare Disease with High Mortality– A Case Report.”, Clinical Case Reports and Clinical Study, 9(5); DOI: 10.61148/2766-8614/JCCRCS/152.
Copyright: © 2023 Amit Mandal. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Fungal endocarditis is a comparatively rare form of endocarditis, accounting for only 1.3% to 6% of all cases of infectious endocarditis [1]. It carries a high mortality rate, as high as 50% [2]. Recommended treatment for fungal Endocarditis is combination of antifungal drugs and surgery.
Introduction:
Fungal endocarditis is a comparatively rare form of endocarditis, accounting for only 1.3% to 6% of all cases of infectious endocarditis [1]. It carries a high mortality rate, as high as 50% [2]. Recommended treatment for fungal Endocarditis is combination of antifungal drugs and surgery.
We report a case of prosthetic valve endocarditis caused by C. parapsilosis and managed with a combination of high dose caspofungin and fluconazole, however ultimately had a fatal outcome because timely source removal was not possible. This case illustrates the importance of both surgical intervention and antifungal antibiotics in treating a case of Fungal endocarditis to obtain a good outcome.
29-year-old female, known case of chronic kidney disease on maintenance haemodialysis, was admitted with complaints of dyspnoea on exertion of one month duration. (NYHA class III, worsened to NYHA class IV over past 2 weeks). Four years back she underwent surgical Aortic valve replacement (Bioprosthetic 23mm EPIC) for Bicuspid Aortic Valve. When she was evaluated for the same at outside hospital, she was told to have prosthetic valve thrombosis and was thrombolysed with streptokinase. However, there was no improvement of her symptoms. She also had low grade fever for last two weeks.
On examination, she was febrile with an axillary temperature of 102° F and a respiratory rate of 28/min, and his blood pressure was 100/80mm Hg in the right arm supine position. Her cardiovascular system examination revealed a mid-sternal scar suggestive of previous sternotomy. On auscultation, a soft first heart sound with high pitched diastolic murmur immediately after A2 with s pansystolic murmur of grade 3/6 at apex was heard. There were no other peripheral signs of infective endocarditis.
Her routine blood investigations revealed. The only lab results showed a low haematocrit, raised ESR, neutrophilic leucocytosis, deranged renal function test. Transthoracic echocardiography revealed a bioprosthetic valve in situ, aortic valve vegetation with aortic root abscess and valve dehiscence with severe Aortic Regurgitation, AML perforation with Mitral Regurgitation. (Figure 1) Her trans-oesophageal revealed stented bioprosthetic valve seen in aortic position with shaggy & thickened leaflets. There was multiple small filamentous mobile structure, suggestive of vegetation. There was an echo free space noted in the posterior aortic annulus and posterior aortic root measuring 27mm X 11mm, suggestive of Aortic root abscess. Tiny filamentous structure was also noted in the aortic end of the abscess, suggestive of Vegetation. (Video 1) She was initially empirically started on ceftriaxone and vancomycin while blood cultures were awaited. Her blood culture grew Candida parapsilosis. She was initiated on Inj.Caspofungin 150mg once daily intravenously. She was transferred to thoracic surgery for surgical intervention. However, she developed refractory hypotension and surgical intervention could not be performed and she succumbed to her illness.
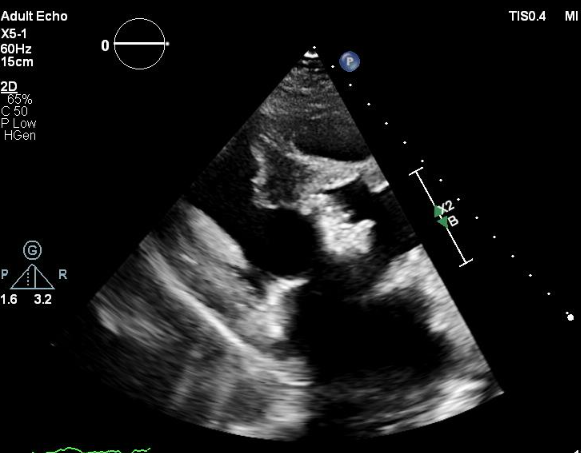
Figure 1: Transthoracic ECHO showing aortic valve vegetation (White arrow) and aortic root abscess (blue arrow)
Discussion:
Fungal endocarditis is a rare form of infective endocarditis with high mortality risk.
The two most common fungi causing endocarditis are species of the genera Candida and Aspergillus. Even though Candida albicans is the most common Candida causing FE, the non-albicans Candida (NAC) species such as C. auris, C. glabrata, C. parapsilosis, C. tropicalis, C. guilliermondii, C. krusei, and C. dubliniensis are largely responsible for in-hospital mortality and morbidity [3]. The common risk factors associated with Fungal endocarditis are underlying cardiac abnormalities, prosthetic heart valves, previous cardiac surgery, intravenous drug abuse and other immunocompromised conditions like hematologic malignancies, recipients of solid organ or hematopoietic cell transplants, Cancer chemotherapy patients [4].The clinical manifestations of Candida endocarditis may be similar to those of bacterial endocarditis, including fever, changing or new heart murmurs, and signs and symptoms of heart failure, making diagnosis more challenging.
Candida species produce biofilm which is an important pathogenic mechanism. The biofilms produced by C. parapsilosis strains associated with invasive disease and they are morphologically different from those produced by C. albicans.[5] Therefore, C. parapsilosis induced endocarditis is more difficult to treat and can recur very late even after completion of therapy.
In the 2016 Infectious Diseases Society of America (IDSA) candidiasis guidelines and the 2015 American Heart Association infective endocarditis guidelines a combined approach with both antifungal agents and valve replacement is recommended for treatment of native and prosthetic valve Candida endocarditis. [6,7]
These guidelines recommend the treatment of Candida PVE with liposomal amphotericin B (3–5 mg/kg/day) in combination with or without flucytosine (25 mg/kg four times daily) or high-dose caspofungin (150 mg daily) as an alternative, along with valve replacement. This must be followed by chronic suppressive therapy with fluconazole (6–12 mg/kg/day) to prevent recurrences. Echinocandins exert their fungicidal activity by inhibiting BDG synthesis and disrupting the fungal cell wall and are the drug of choice against most Candida species. [8]
Despite the combination of medical therapy and surgical intervention, the mortality rate for C. parapsilosis endocarditis is as high as 40% [9].
Conclusion:
Candida IE is a rare form of IE with a high propensity to involve implanted prosthetic valves and implanted cardiac devices. This case focuses on the presentation of Candida parapsilosis IE with subsequent imaging findings of this rare disease. In addition, this case highlights that high index of suspicion is required for successful diagnosis and treatment of this condition.